Lost Lessons – Succumbing to the Inescapable Food Coma
By Dana Kim 金娥凜

*Yawn*
Oh no, your teacher stares at you. You rub your eyes, trying to focus on the differentiation problem your teacher asked you to solve.
You start to think, is it the bowl of noodles I had for lunch? Why is it that a food coma hits us so hard every time after lunch?
Common Misconception About Food Coma
Traditionally, it is believed that sleepiness after a meal is due to the redistribution of blood flow. We think that blood rushes through the stomach and intestines to facilitate digestion, resulting in a reduction in blood and oxygen supplies to our brain and hence the induction of post-meal sleepiness, medically known as postprandial somnolence [1].
Post-Meal Hormonal Change and Food Coma
So, what could be the possible reasons behind food coma? With the postprandial increase in insulin level as an example, feeding can promote or inhibit the secretion of a lot of hormones to maintain homeostasis. Such hormonal changes can also reduce the desire for food intake by introducing a feeling of satiety. It has been suggested that the hormones involved may simultaneously affect the sleeping centers in the brain and contribute to food coma (footnote 1) [1, 2]. We will examine two (of the many) examples – melatonin and orexin.
In addition to its role in regulating gastrointestinal motility [3], melatonin is commonly known as a hormone that regulates sleep-wake cycle – high levels of melatonin induce sleep. This has been shown by administrating melatonin to animals and humans in previous studies [2]. In fact, the gut increases the synthesis of melatonin considerably after meal consumption, so such increase is considered to be a contributing factor to food coma [2].
For orexin, it is known to be a hormone which promotes hunger, along with wakefulness, presumably through increasing the firing rate of neurons in an arousal center in the hypothalamus [2], which was hypothesized to work by inhibiting the sleep centers [1]. Therefore, the reduction of orexin after a meal may contribute to the sleep-inducing effect by leaving off the inhibition of the sleep centers [2].
Consider the Bigger Picture: Interactions Between Brain Centers
While some scientists incline to attribute the cause of food coma to the action of certain hormones, some take a further step back [1]. On top of the idea that the hunger-satiety axis modulates the sleep-wake axis, this view emphasizes the interaction between brain centers in the hypothalamus, and hormones are considered as just messengers that facilitate communication between organs.
As illustrated by the example of orexin above, there are four major centers in the hypothalamus that affect satiety and drowsiness. They can be simplified as the hunger, satiety, arousal and sleep centers. Hunger often comes with wakefulness; the hunger center is hypothesized to stimulate the arousal center and inhibit the sleep center. The arousal center itself works by inhibiting the sleep center, too. However, in the state of satiety, the satiety center inhibits the hunger center so everything in the pathway becomes the opposite and drowsiness occurs. The interactions are summarized in Figure 1.
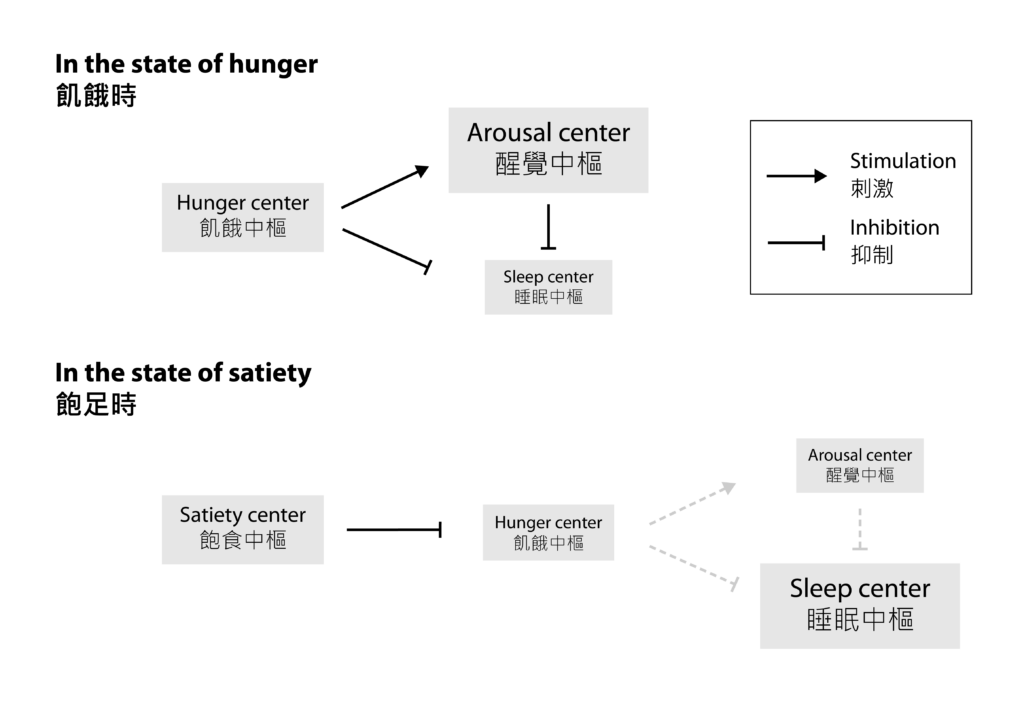
Figure 1 The interactions between the four brain centers before and after a meal
So, it is useful to understand what would lead to the feeling of satiety, which intertwines with the occurrence of post-meal sleepiness. In fact, our body judges whether we should feel full by our energy level and by the physical conditions of the stomach [1].
To know whether we are replenished with energy after a meal, arcuate nucleus (ARC; footnote 2) in the hypothalamus detects the increase in the level of a blood-borne metabolite, malonyl-CoA, whose level correlates with that of ATP (“energy”). Having combined other metabolic signals, ARC can stimulate the satiety center and inhibit the hunger center through hormonal regulation. This contributes to the feelings of satiety and drowsiness.
Meanwhile, our stomach should be stuffed with food for quite a while after eating. Vagus nerve branches can sense the gastric distension and delayed gastric emptying, which in turn lead to the release of some other gut hormones that stimulate the satiety center by their own actions and through vagal stimulation. This eventually yields the same feelings of being full and sleepy. Furthermore, this can account for the reason why solid food could induce greater drowsiness than liquid food, which is because solid food can cause greater gastric distension and further delay gastric emptying.
Food Coma in the Light of Evolution
So now, you may all be wondering – is it necessary for the satiety response to link to drowsiness? All it does it gets us into trouble for dozing off during class, right? True, but evolutionary biology suggests that there might be a reason behind post-meal sleepiness.
To understand, we need to view this phenomenon in the Darwinian context – any suboptimal effort allocation can result in a selection disadvantage [4]. For a species to survive in natural selection, they must spend their limited energy and effort wisely.
Speaking of these, some researchers speculated that digestion is a demanding metabolic process that requires focused effort and energy expenditure [2]. In response to that, our body may choose to temporarily lower its sensitivity to external stimuli to let our body “concentrate” on digestion by reducing energy and effort demands [2]. This could be the reason why we suddenly lose the vigor to hunt for extra calories.
Another plausible reason is that post-meal sleepiness may help consolidate what we learned from the circumstances that led to energy acquisition [2]. The brain is known to be plastic, or flexible, as neurons can rewire themselves to enable more effective communication. This serves as the basis of learning and memory. It has been proposed that neuronal connections can be remodeled and strengthened during sleep [5], so sleep is long suspected to be a process that facilitates learning. With this concept in mind, post-meal sleep was suggested to subconsciously reinforce what you learn from the energy-acquiring experience before the meal – say, hunting. It prepares you for future opportunities to acquire energy [2].
So, food coma could actually give us an edge in natural selection!
Unraveling the Mystery Between Feeding Biology and Sleep
Research studies on physiology and neuroscience have unveiled layers of mysteries of food coma by deciphering the functions of different hormones and brain parts. However, to this day, we are still unable to confirm why or how we get food coma confidently. Similar to many other scientific topics, like why we sleep, there are still many unanswered questions regarding the potential link between feeding biology and sleep.
1 Editor’s note: Recall that one hormone can target multiple organs in hormonal coordination (cf. nervous coordination), so it is common for a hormone to perform multiple functions in different organs.
2 Nucleus: In the central nervous system, the word “nucleus” is used to describe a group of neurons that are located in a defined anatomical position.
References:
[1] Kim SW, Lee BI. Metabolic state, neurohormones, and vagal stimulation, not increased serotonin, orchestrate postprandial drowsiness. Biosci Hypotheses. 2009;2(6):422-427. doi:10.1016/j.bihy.2009.07.008
[2] Bazar KA, Yun AJ, Lee PY. Debunking a myth: neurohormonal and vagal modulation of sleep centers, not redistribution of blood flow, may account for postprandial somnolence. Med Hypotheses. 2004;63(5):778-782. doi:10.1016/j.mehy.2004.04.015
[3] Chen CQ, Fichna J, Bashashati M, Li YY, Storr M. Distribution, function and physiological role of melatonin in the lower gut. World J Gastroenterol. 2011;17(34):3888-3898. doi:10.3748/wjg.v17.i34.3888
[4] Gregory TR. Understanding Natural Selection: Essential Concepts and Common Misconceptions. Evolution (N Y). 2009;2(2):156-175. doi:10.1007/s12052-009-0128-1.
[5] Frank MG, Issa NP, Stryker MP. Sleep enhances plasticity in the developing visual cortex. Neuron. 2001;30(1):275-287. doi:10.1016/s0896-6273(01)00279-3